Introduction
Peripheral Arterial Disease (PAD) is a common circulatory problem characterized by narrowed arteries that reduce blood flow to the limbs, particularly the legs. This condition often leads to debilitating symptoms such as leg pain, cramping, and difficulty walking. As PAD progresses, it can severely impact a patient’s quality of life, potentially resulting in severe complications, including ulcers and limb amputation. However, advancements in medical technology have introduced effective endovascular procedures that can significantly improve circulation in patients suffering from PAD. This article will explore how these minimally invasive procedures work, their benefits, and their role in managing PAD.
Understanding Peripheral Arterial Disease
What is Peripheral Arterial Disease?
Peripheral Arterial Disease (PAD) manifests through a variety of symptoms, primarily due to reduced blood flow to the legs and feet. Understanding these symptoms is crucial for early diagnosis and effective management of the condition. Here, we delve into some of the most common symptoms associated with PAD: intermittent claudication, rest pain, weak or absent pulses, leg ulcers, and gangrene.
1. Intermittent Claudication
Intermittent claudication is characterised by pain, cramping, or heaviness in the legs or buttocks during physical activities such as walking, climbing stairs, or exercising. This discomfort occurs due to insufficient blood flow to the muscles, which need more oxygen during exertion.
Symptoms:
- The pain typically manifests in the muscles of the calves, thighs, or buttocks.
- Symptoms often begin after a certain distance is walked or a specific level of exertion is reached.
- Pain usually resolves within a few minutes of rest, as blood flow returns to normal.
- Patients may note that they can walk shorter distances over time as the condition progresses.
Mechanism: The underlying cause of intermittent claudication is atherosclerosis, where fatty deposits narrow the arteries, reducing blood flow. As physical activity increases, the demand for oxygen in the muscles rises, and the narrowed arteries cannot supply enough oxygenated blood, resulting in pain.
Management: Intermittent claudication can often be managed through lifestyle changes, such as quitting smoking, engaging in supervised exercise programs, and medications to improve circulation. In more severe cases, interventional procedures may be necessary.
2. Rest Pain
Definition: Rest pain refers to a sensation of pain or discomfort in the feet or toes while resting, particularly at night when lying flat. This symptom often indicates more advanced PAD and significantly impacts the quality of life.
Symptoms:
- Patients may experience burning or aching pain in the feet or toes, which can be more pronounced at night.
- The pain may be relieved by hanging the legs over the edge of the bed or walking around.
- Patients may struggle to find a comfortable position due to the persistent discomfort.
Mechanism: Rest pain occurs when blood flow to the extremities is severely restricted, causing pain even without exertion. This is often a sign that the disease has progressed significantly and may require more aggressive treatment.
Management: Addressing rest pain typically involves a combination of lifestyle modifications and medical management. Patients may be prescribed medications to improve blood flow or manage pain. In some cases, surgical interventions such as angioplasty or bypass surgery may be necessary to restore adequate blood flow.
3. Weak or Absent Pulses
Definition: Reduced blood flow due to PAD can lead to weak or absent pulses in the legs and feet. This symptom is often identified during a physical examination by a healthcare professional.
Symptoms:
- Weak or diminished pulses in the femoral, popliteal, and dorsalis pedis arteries can indicate impaired blood flow.
- Patients may also experience coolness or temperature differences between the affected leg and the other leg.
- Changes in skin color (pale or bluish tint) may be observed, particularly in the toes and feet.
Mechanism: The presence of weak or absent pulses signifies that the arteries supplying blood to the legs are significantly narrowed or blocked. This condition reflects the severity of PAD and can indicate an increased risk for severe complications.
Management: The management of weak or absent pulses involves a thorough vascular assessment and may require imaging studies to evaluate the extent of arterial disease. Treatment options may include lifestyle changes, medications, and surgical interventions aimed at restoring blood flow.
4. Leg Ulcers
Definition: Leg ulcers are non-healing sores or wounds on the feet or legs, often resulting from inadequate blood flow and poor wound healing associated with PAD.
Symptoms:
- Ulcers may appear as open sores or wounds that do not heal over time.
- Common sites for leg ulcers include the feet, particularly around the ankles and toes.
- Patients may experience pain, swelling, and signs of infection, such as redness, warmth, and discharge.
Mechanism: Insufficient blood flow hampers the body’s natural healing processes, making it difficult for wounds to heal. As a result, even minor injuries or pressure sores can develop into chronic ulcers.
Management: Treating leg ulcers typically involves addressing the underlying PAD through lifestyle modifications and medical interventions. Proper wound care, including cleaning, dressing, and managing infection, is essential. Advanced treatments, such as hyperbaric oxygen therapy or endovascular procedures, may be required for non-healing ulcers.
5. Gangrene
Definition: Gangrene is a severe condition resulting from tissue death due to a lack of blood supply. It can lead to serious complications, including limb amputation if not addressed promptly.
Symptoms:
- Early signs of gangrene may include severe pain, swelling, and discoloration (black or brown) of the affected area.
- As the condition progresses, the skin may become cold and numb, and a foul odor may be present due to tissue necrosis.
- Patients may also experience systemic symptoms such as fever and chills.
Mechanism: Gangrene occurs when the blood supply to a particular area is severely compromised, leading to tissue death. In PAD, the risk of gangrene is heightened due to prolonged ischemia (lack of blood flow), particularly in individuals with advanced disease or poorly managed diabetes.
Management: Prompt medical intervention is crucial in cases of gangrene. Treatment often involves antibiotics to combat infection, surgical removal of dead tissue (debridement), and restoring blood flow through surgical or endovascular procedures. In severe cases, amputation may be necessary to prevent the spread of infection.
Risk Factors for PAD
Several risk factors contribute to the development of PAD, including:
- Age: The risk increases with age, particularly in individuals over 50.
- Diabetes: Diabetic patients are at a higher risk due to potential damage to blood vessels.
- Smoking: Tobacco use significantly increases the likelihood of developing PAD.
- High Blood Pressure: Hypertension can contribute to arterial damage and narrowing.
- High Cholesterol: Elevated cholesterol levels can lead to plaque buildup.
- Family History: A family history of cardiovascular diseases may elevate risk.
Endovascular Procedures for PAD
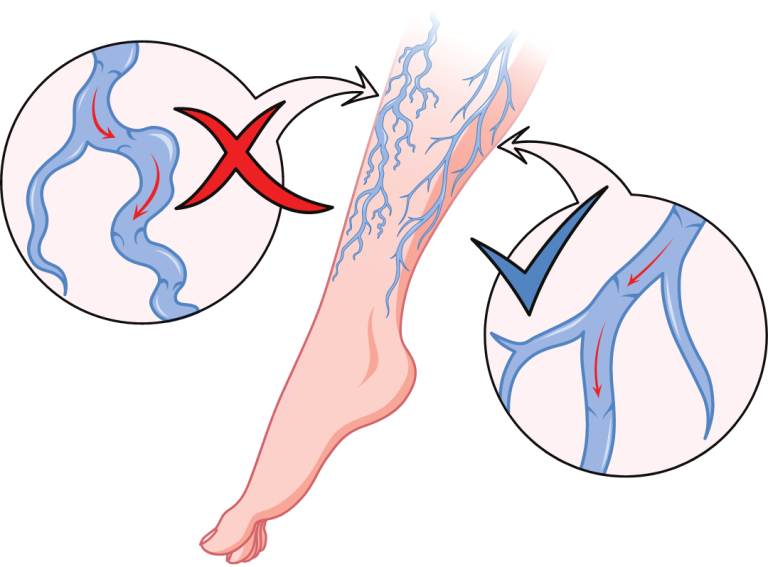
Endovascular procedures are minimally invasive techniques used to treat blockages in the arteries, improving blood flow to affected areas. These procedures can provide significant relief for patients suffering from PAD. The most common endovascular procedures for PAD include angioplasty, stenting, and atherectomy.
Angioplasty
What is Angioplasty?
Angioplasty is a procedure that opens narrowed or blocked arteries to improve blood flow. The procedure is typically performed under local anesthesia and involves the following steps:
- Accessing the Artery: A small incision is made in the skin, usually in the groin area, to access the femoral artery. A catheter (a thin, flexible tube) is inserted into the artery.
- Guiding the Catheter: Using fluoroscopy (real-time X-ray imaging), the interventional radiologist guides the catheter through the arteries to the site of the blockage.
- Inflating the Balloon: Once the catheter reaches the narrowed section, a small balloon at the catheter’s tip is inflated. This balloon compresses the plaque against the artery walls, widening the artery and improving blood flow.
- Deflating the Balloon and Removing the Catheter: The balloon is then deflated, and the catheter is removed.
- Post-Procedure Monitoring: Patients are monitored for a short period before being discharged, often on the same day.
Benefits of Angioplasty
- Minimally Invasive: Angioplasty requires only a small incision, leading to less pain, minimal scarring, and a shorter recovery time compared to open surgery.
- Quick Recovery: Most patients can return to normal activities within a few days.
- Immediate Symptom Relief: Many patients experience immediate relief from symptoms, such as leg pain or cramping, following the procedure.
Stenting
What is Stenting?
Stenting is often performed in conjunction with angioplasty. A stent is a small mesh-like device that is placed in the artery to help keep it open after angioplasty. The procedure involves the following steps:
- Placement of the Stent: After angioplasty, a stent mounted on a balloon catheter is positioned at the site of the blockage.
- Inflating the Balloon: The balloon is inflated to expand the stent against the artery wall, securing it in place.
- Deflating and Removing the Balloon: The balloon is then deflated, and the catheter is removed, leaving the stent in place to help maintain the newly opened artery.
Benefits of Stenting
- Keeps Arteries Open: Stents provide structural support to the artery, reducing the risk of re-narrowing (restenosis) and maintaining improved blood flow.
- Long-Term Solution: Stenting can provide long-term relief from symptoms and improve overall circulation.
- Minimal Recovery Time: Similar to angioplasty, stenting is minimally invasive, allowing for quick recovery and return to normal activities.
Atherectomy
What is Atherectomy?
Atherectomy is a procedure that involves the removal of plaque buildup from the artery using a specialized catheter with a rotating blade or laser. This procedure can be performed in conjunction with angioplasty and stenting. The steps involved in atherectomy include:
- Accessing the Artery: As with angioplasty, a small incision is made, and a catheter is inserted into the femoral artery.
- Guiding the Catheter: The catheter is guided to the blockage under fluoroscopic guidance.
- Removing Plaque: The rotating blade or laser at the tip of the catheter removes the plaque from the artery wall, allowing for improved blood flow.
- Post-Procedure Monitoring: Similar to other endovascular procedures, patients are monitored for a short time post-procedure.
Benefits of Atherectomy
- Effective for Complex Lesions: Atherectomy can be particularly effective for complex lesions, such as those involving heavily calcified plaque.
- Improved Angioplasty Outcomes: By removing plaque before angioplasty, atherectomy can enhance the outcomes and longevity of the angioplasty and stenting procedures.
- Minimally Invasive: Like angioplasty and stenting, atherectomy is a minimally invasive procedure with quick recovery times.
Benefits of Endovascular Procedures in Managing PAD
Endovascular procedures have transformed the management of Peripheral Arterial Disease, offering several benefits over traditional open surgical approaches:
1. Minimally Invasive Nature
- Less Trauma: Endovascular procedures require only small incisions, resulting in less trauma to the body compared to open surgeries that require larger incisions.
- Reduced Scarring: Smaller incisions lead to minimal scarring, improving cosmetic outcomes.
2. Shorter Recovery Times
- Faster Recovery: Most patients can return home the same day as the procedure, and many are able to resume normal activities within a few days.
- Lower Hospitalization Rates: The minimally invasive nature of endovascular procedures often reduces the need for prolonged hospital stays.
3. Immediate Symptom Relief
- Quick Improvement: Many patients experience immediate relief from symptoms such as leg pain, cramping, and difficulty walking after undergoing endovascular treatments.
- Enhanced Quality of Life: The restoration of blood flow can significantly improve patients’ quality of life, allowing them to engage in daily activities without discomfort.
4. Reduced Risks and Complications
- Lower Risk of Infection: The risk of infection is reduced due to the smaller incisions and the minimally invasive nature of the procedures.
- Fewer Complications: Endovascular procedures have lower complication rates compared to open surgeries, leading to safer outcomes for patients.
5. Repeatability
- Multiple Treatments Possible: If necessary, endovascular procedures can be repeated for recurrent blockages, allowing for ongoing management of PAD.
6. Preservation of Arterial Function
- Preservation of Blood Flow: Endovascular techniques aim to restore blood flow while preserving as much healthy arterial tissue as possible.
- Functional Improvement: Restoring blood flow can enhance the overall function of the affected limb, reducing the risk of complications associated with chronic PAD.
Conclusion
Peripheral Arterial Disease is a significant health concern that can lead to debilitating symptoms and complications. Endovascular procedures such as angioplasty, stenting, and atherectomy offer effective, minimally invasive options for improving circulation in patients with PAD. These procedures provide immediate symptom relief, promote faster recovery, and minimize the risks associated with traditional surgical interventions. As advancements in endovascular techniques continue to evolve, patients with PAD can expect improved outcomes and enhanced quality of life.
If you or someone you know is experiencing symptoms of PAD, it is essential to consult with an interventional radiologist or vascular specialist. Early diagnosis and intervention can significantly impact the management of PAD and reduce the risk of severe complications.